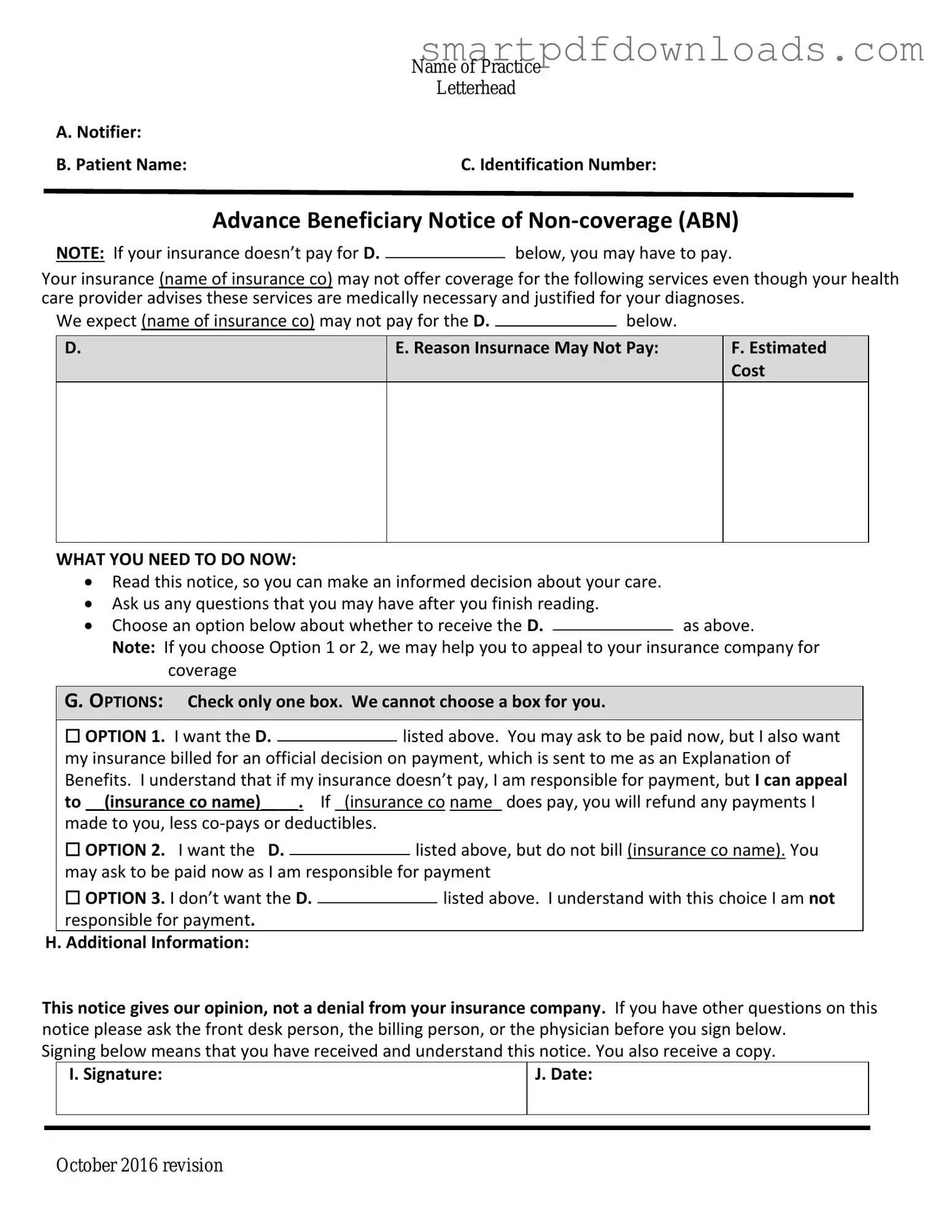
Advance Beneficiary Notice of Non-coverage Form
The Advance Beneficiary Notice of Non-coverage (ABN) is a form used in the Medicare program. It informs beneficiaries that a service or item may not be covered by Medicare. Understanding this form can help beneficiaries make informed decisions about their healthcare options.
Edit Advance Beneficiary Notice of Non-coverage Online
Advance Beneficiary Notice of Non-coverage Form
Edit Advance Beneficiary Notice of Non-coverage Online
Edit Advance Beneficiary Notice of Non-coverage Online
or
⇓ PDF File
Finish the form and move on
Edit Advance Beneficiary Notice of Non-coverage online fast, without printing.