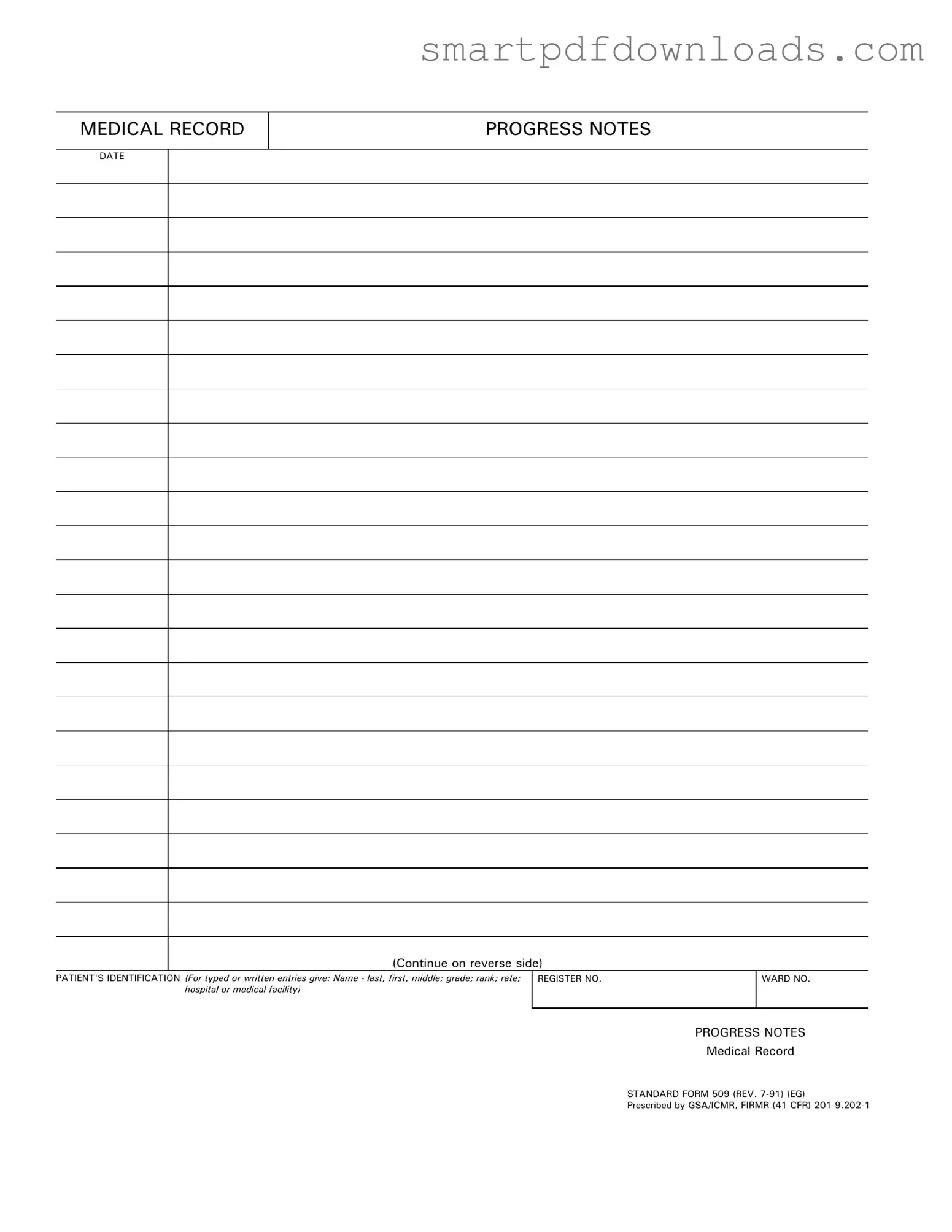
Progress Notes Form
The Progress Notes form is a vital component of medical records, used to document patient care and treatment over time. This standardized form allows healthcare providers to record essential information, including the patient's identification, date of service, and details of the medical progress. By maintaining accurate and comprehensive progress notes, medical professionals ensure continuity of care and support effective communication within the healthcare team.
Edit Progress Notes Online
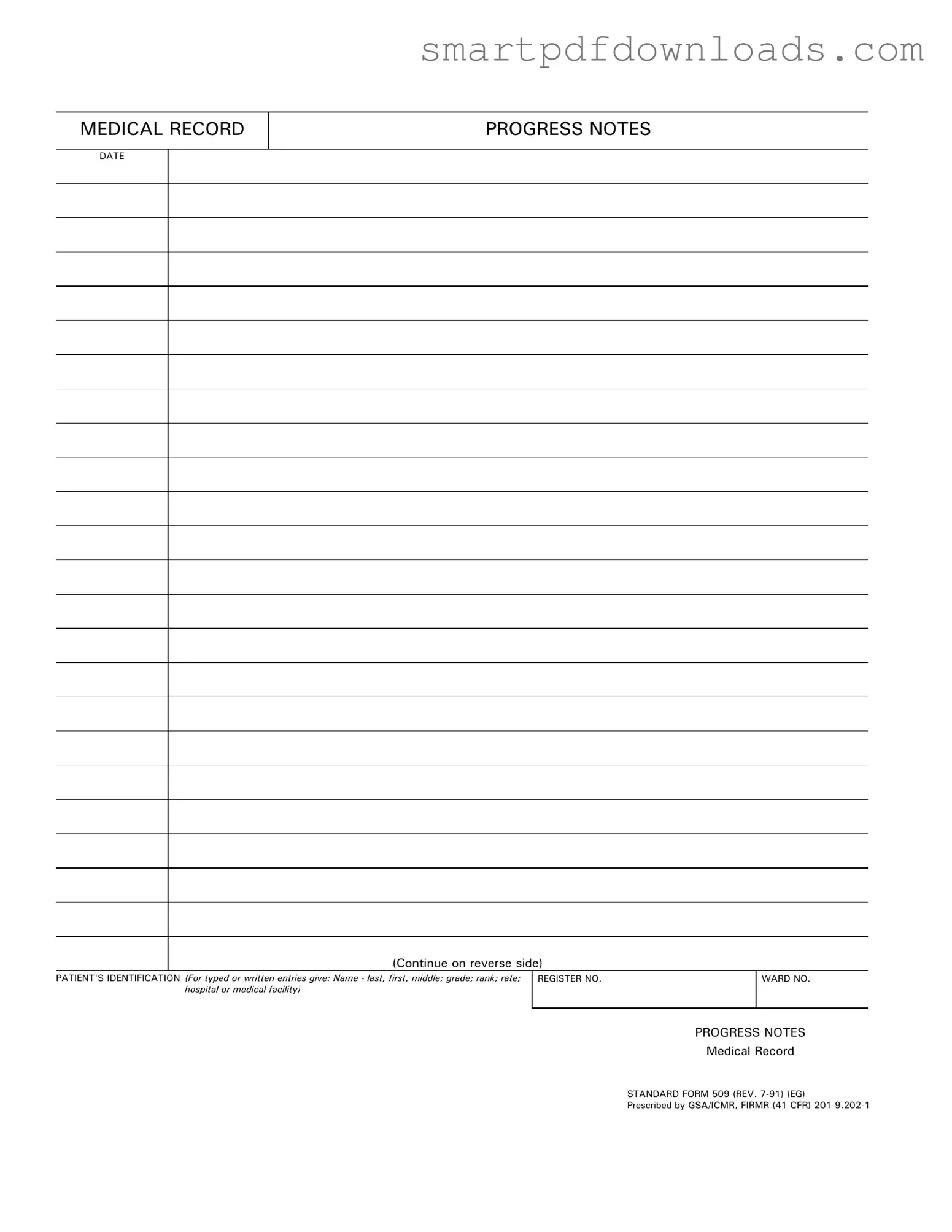
Progress Notes Form
Edit Progress Notes Online
Edit Progress Notes Online
or
⇓ PDF File
Finish the form and move on
Edit Progress Notes online fast, without printing.